Background
This blog explores the transformative potential of Artificial Intelligence (AI) in streamlining clinical workflows. It delves into real-world success stories showcasing how AI is being used to improve efficiency, reduce errors, and enhance patient care. Furthermore, it outlines best practices for implementing AI solutions in clinical settings, addressing key considerations such as data privacy, ethical implications, and the importance of human-AI collaboration.
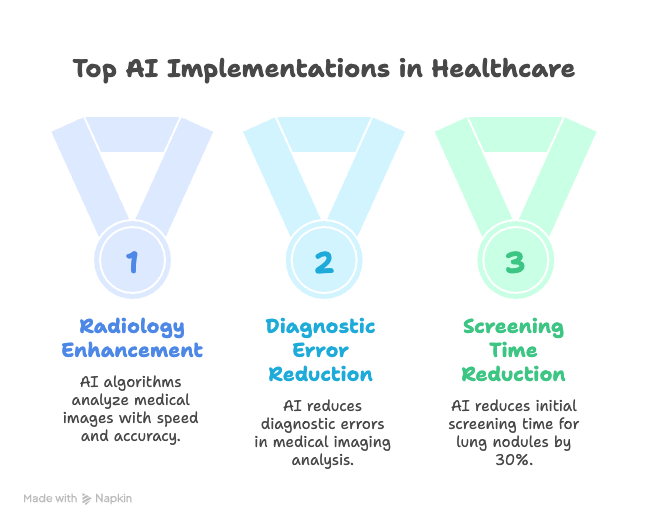
Success Stories: AI in Action
Several healthcare organizations have already witnessed significant improvements by integrating AI into their clinical workflows. Here are a few notable examples:
- Radiology Enhancement: AI algorithms are being used to analyze medical images (X-rays, CT scans, MRIs) with remarkable speed and accuracy. This assists radiologists in identifying anomalies, prioritizing urgent cases, and reducing diagnostic errors. For instance, a hospital in the UK implemented an AI-powered system for detecting lung nodules on chest X-rays, resulting in a 30% reduction in the time required for initial screening.
- Automated Prior Authorization: The prior authorization process for medications and procedures can be incredibly time-consuming for both clinicians and administrative staff. AI-powered solutions can automate much of this process by analyzing patient data, insurance policies, and clinical guidelines to determine eligibility and generate necessary documentation. This reduces administrative burden and accelerates patient access to needed care. One case study showed a 40% reduction in prior authorization processing time after implementing an AI solution.
- Predictive Analytics for Patient Deterioration: AI models can analyze patient data from electronic health records (EHRs) and wearable devices to predict the likelihood of patient deterioration, such as sepsis or cardiac arrest. This allows clinicians to proactively intervene and prevent adverse events. A hospital in the US reported a 25% reduction in mortality rates for patients with sepsis after implementing an AI-powered predictive analytics system.
- Virtual Assistants for Patient Engagement: AI-powered virtual assistants can provide patients with personalized support, answer their questions, and remind them about appointments and medications. This improves patient engagement and adherence to treatment plans. A study found that patients who used a virtual assistant for diabetes management had significantly better blood sugar control compared to those who did not.
Best Practices for AI Implementation
While the potential benefits of AI in healthcare are significant, successful implementation requires careful planning and execution. Here are some best practices to consider:
- Define Clear Objectives: Before implementing any AI solution, it is crucial to define clear and measurable objectives. What specific clinical workflow are you trying to improve? What are the desired outcomes? Having well-defined objectives will help you select the right AI solution and track its performance.
- Ensure Data Quality and Accessibility: AI algorithms are only as good as the data they are trained on. It is essential to ensure that your data is accurate, complete, and accessible. This may involve data cleaning, standardization, and integration across different systems.
- Address Data Privacy and Security: Patient data is highly sensitive, and it is crucial to protect it from unauthorized access and use. Implement robust security measures to comply with HIPAA and other relevant regulations. Ensure that patients are informed about how their data is being used and have the opportunity to opt out.
- Prioritize Human-AI Collaboration: AI should be viewed as a tool to augment human capabilities, not replace them. Clinicians should always have the final say in patient care decisions. Provide adequate training to clinicians on how to use AI tools effectively and interpret their results.
- Address Ethical Considerations: AI raises a number of ethical considerations, such as bias, transparency, and accountability. Ensure that your AI solutions are fair, unbiased, and transparent. Establish clear lines of accountability for AI-related decisions.
- Monitor and Evaluate Performance: Continuously monitor and evaluate the performance of your AI solutions to ensure that they are meeting your objectives. Track key metrics such as accuracy, efficiency, and patient outcomes. Use this data to identify areas for improvement and refine your AI models.
- Foster a Culture of Innovation: Encourage experimentation and innovation with AI. Create a supportive environment where clinicians and data scientists can collaborate to develop and implement new AI solutions.
Conclusion
AI has the potential to revolutionize clinical workflows, improve patient care, and reduce healthcare costs. By following these best practices and learning from the success stories of others, healthcare organizations can successfully implement AI solutions and unlock their full potential. The key is to approach AI implementation strategically, focusing on clear objectives, data quality, human-AI collaboration, and ethical considerations. As AI technology continues to evolve, it will undoubtedly play an increasingly important role in shaping the future of healthcare.